Zvandiri
Youth living with HIV are the hardest to treat and are most at risk for transmission of the virus, but standard healthcare approaches fail them.
The Idea
Peer Therapy for Adolescents Living with HIV


Total Investment
1950000
Grants
0
Equity/SAFE
0
Debt/Convertible Debt
Funded Since
2021
Geography
Sector
Structure
The Mission
HIV+ youth in Africa survive and thrive.
How It Works
Zvandiri trains HIV-positive adolescents as peer counselors for other HIV-positive youth. These government-employed healthcare workers connect with peers through visits and messaging, escalating cases to medical professionals when needed. The program improves treatment adherence, reduces viral loads to undetectable levels, and materially improves mental health outcomes.
The Dream
African health systems deliver HIV and mental health care to young people through trained peer counselors integrated into clinics and surrounding communities.
Why We're In
2.4 million young people are HIV+ and compared to HIV+ adults, they are harder to diagnosis and to treat. The pandemic won’t end if we can’t reach them. Zvandiri has an excellent solution, designed for delivery by governments from day one. Rigorous studies showed spectacular viral load reductions—low enough to eliminate transmission to others. It is now recommended by WHO as the standard of care, and Zvandiri is working with governments in 14 countries.
Delivery
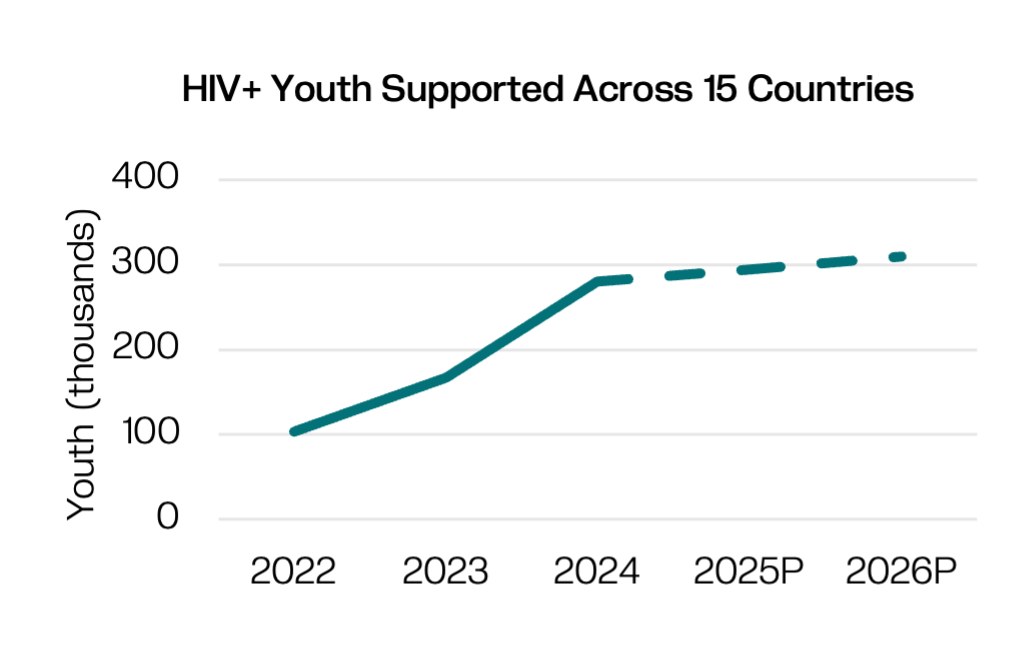
Zvandiri saw incredible growth in HIV+ youth reached across Zimbabwe, and now expansion has slowed as the 14 other Thrive95 countries work to secure funding to scale the program.
Impact
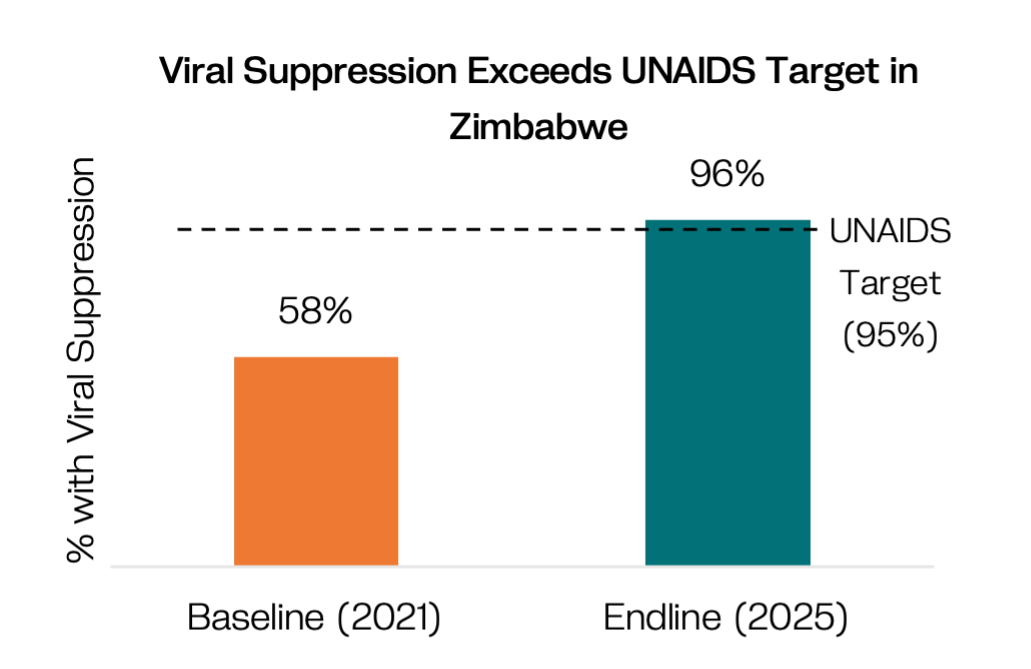
The most recent study of government-led delivery in Zimbabwe showed 96% of HIV+ youth were virally suppressed, which exceeds the UNAIDS target of 95%.
The Model
A solution that works and can scale.
Peer Counselors
Recruit and train subset of HIV+ youth to become peer counselors.
Counseling
Peer counselors deliver services in homes, support groups, facilities and via phone nudges.
Health Systems Integration
Embed everything into existing health structures and policy.
Potential for Impact at Scale
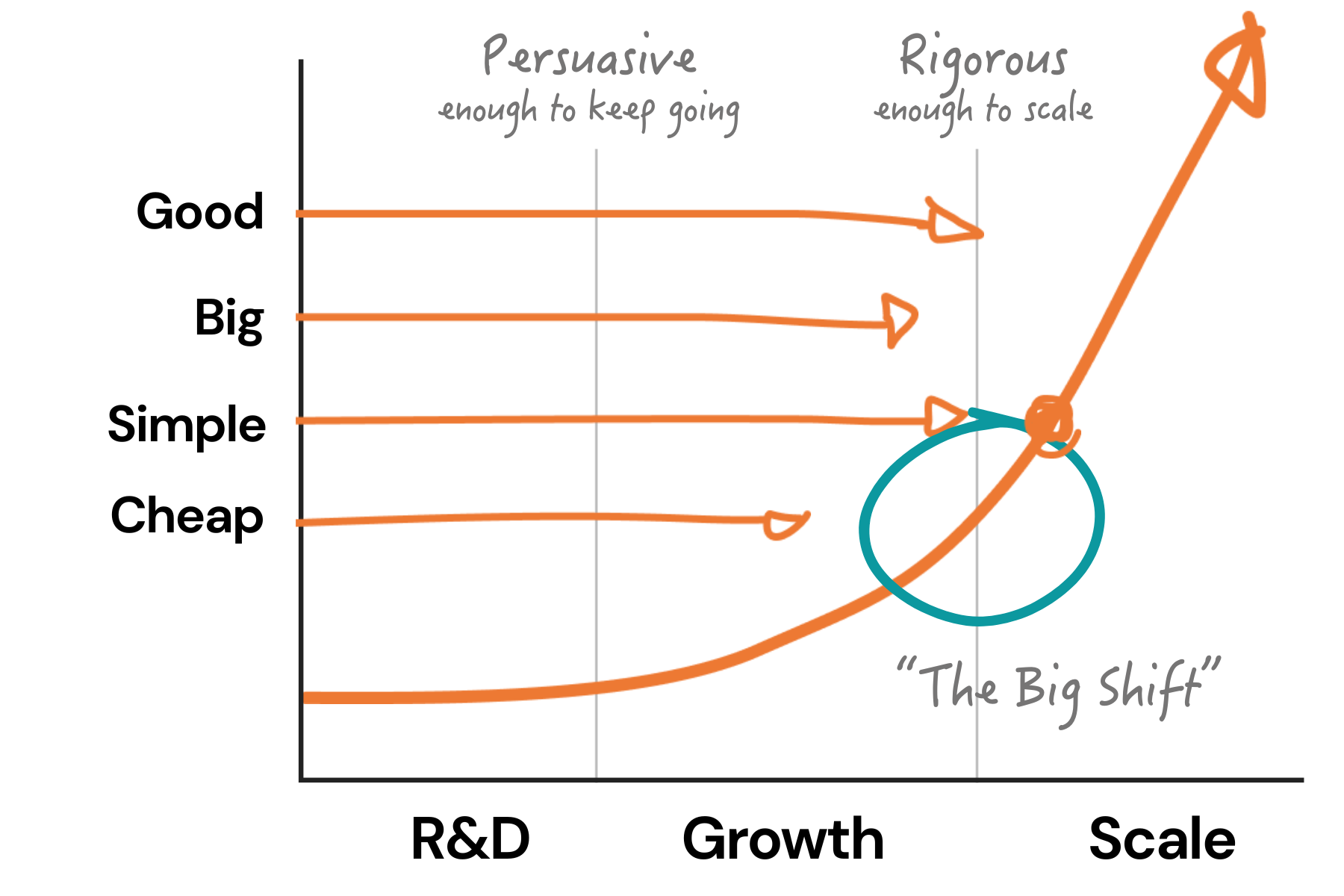
Mulago uses four criteria to gauge potential for exponential impact. The model must be:
This is about impact. Zvandiri has rigorous evidence from a 2016-2019 RCT in Zimbabwe that its model improves adherence to treatment protocols: 75% of Zvandiri youth were virally suppressed compared to 64% who received standard HIV care. A 2nd RCT showed a 60%+ reduction in anxiety and depression. And the most recent independent study showed that results are excellent when government is delivering and paying: 96% of Zvandiri youth were virally suppressed (baseline was 58%), surpassing the global UNAIDS target of 95%. Zvandiri is planning to conduct external process and impact evaluations in 3-4 countries, building evidence of fidelity when delivered by other governments.
This is about scope. Kids, adolescents, and young adults living with HIV are the hardest to treat and 84% of them live in Africa. In total numbers that’s ~2M+ young people, which might sound low but without reaching them there is no chance in ending the HIV epidemic. Zvandiri is making progress in 15 countries, though the collapse of Big Aid is an unexpected constraint that requires all countries to fund more immediately from domestic budgets. Understanding the potential for continued expansion requires more time and evidence.
This is about the ability for Ministries of Health to deliver the model. Zimbabwe’s rollout proved government can deliver this at scale, and Zvandiri has invested in digital tools to ease delivery and strengthen data. They also co-developed, in partnership with the WHO and UNICEF, the “Thrive95” framework to strengthen health systems to support HIV+ youth. 14 other countries are using Thrive95 to plan for government delivery without direct Zvandiri support, but we don’t yet know if the full model will be deployed in all countries.
This is about the cost of the product. In Zimbabwe, the intervention costs $26/child/year, affordable for an intervention that so successfully reaches HIV+ youth, a population who is very hard to reach. The government’s willingness to pay shows it is cheap enough. They are delivering in 13 districts with a combination of taxes and support from Global Fund and are prepared to expand if PEPFAR funding ends, convinced in part by the savings on future HIV treatment. Zvandiri’s lighter-touch technical assistance in other Thive95 countries supports government to better understand costs and willingness to pay.
Zvandiri is actively scaling through government in Zimbabwe, and a host of other countries are starting to adopt the model.
Our Take
Zvandiri's evidence is rigorous, and the outcomes are awesome: despite this being the hardest to reach HIV+ age-group, they have surpassed the UNAIDS 95% target in Zimbabwe. The model is simple enough for governments to deliver at scale and WHO's recommendation of the Zvandiri protocol unlocked initial funding from Big Aid while spurring adoption in 14 high-burden countries. And now in the face of Big Aid’s collapse, the program's cost is still low enough for Zimbabwe to sustain beyond donor funding, but time will tell if it’s cheap enough for expansion countries to reach national-level coverage.
Are you a serious funder and want to learn more?
This is just a snapshot of what we know about the organization. If you're an investor or funder that might send some serious dough their way, we're always delighted to share more. Reach out and we'll connect you with the right person on our team.
*this is not monitored for funding requests.


.JPG)




.jpeg)


